
Experts at Cincinnati Children's shed new light on molecular mechanisms involved in becoming food allergen sensitized that illuminates the 'hygiene hypothesis'
CINCINNATI, Nov. 12, 2025 /PRNewswire/ -- Clinicians who treat allergies have known for years that children tend to be less likely to suffer severe food allergy problems if they grow up with pets in the house. Now, experts have new information about how that protection works—and the results may have wide-reaching implications for controlling allergy risk.
The study, published online Nov. 11, 2025, in the journal Allergy, was led by a team of 19 experts in asthma, biomedical informatics, genetics, immunology and other fields at Cincinnati Children's.
The team deeply analyzed the genetic activity of antibodies produced by 147 children with atopic dermatitis (AD), a skin condition that increases a child's risk of later developing severe allergic disease. The team looked for signs of somatic hypermutation (SHM), an immune process that pushes B cells in the immune system to produce more intense immune reactions.
Within the large group, some children exhibited food allergen sensitivities (such as to peanuts, milk, or eggs), but others did not. The team confirmed that children with sensitivity to foods had B cells in their immune systems that produced high amounts of IgE, an antibody type that drives severe allergic reactions.
Then they found something unexpected. Children with food allergen sensitivities actually had less somatic hypermutation (SHM) of IgE genes.
"At least for children in this cohort, under six years old, food allergic sensitization looks more like a suppressed immune system instead of an overactive one, as most immunologist would naturally assume," says Krishan Roskin, PhD, corresponding author for the study. "The developing immune system of young children with food sensitivities seems to lag behind other children by over three years."
Yet when a dog was in the home, this effect appears to be blunted. Exposure to the dogs seems to restore normal IgE immune development.
However, the protective effects of having a pet in the house appear limited to dogs, the report states.
These findings may help address a debate about the 'hygiene hypothesis' which contends that growing up in less-clean environments generally reduces allergy risk.
"Our findings are consistent with the hygiene hypothesis," Roskin says. "It sheds light on how less-sterile environments act mechanistically on the developing immune system in a positive way. This is particularly exciting given that new drugs are being tested in clinical trials than stimulate the immune system in a similar way."
Notably, the study's findings also are limited to food reactions. None of B cell changes documented by the research team were connected to airborne allergies such as plant pollens or molds.
Looking forward, Roskin plans to present these findings at future medical and scientific conferences. More research is needed to extend these results beyond atopic dermatitis to other cohorts and people with clinically confirmed food allergy.
About the Study
Co-authors from Cincinnati Children's and the University of Cincinnati also included Kristina Preusse, Brittany Cain, Rebecca Hotz, Parthav Gavini, Zhenyu Yuan, Christopher Ahn, Hee-Woong Lim, and Rhett Kovall. Contributors also included members of the Xavier University Department of Chemistry, the University of London, and King's College London.
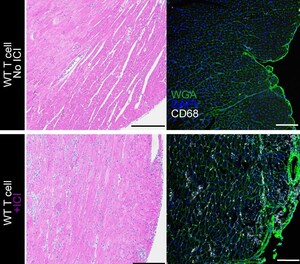
Research work for this study also was supported by these core facilities at Cincinnati Children's: the Transgenic Animal and Genome Editing Facility, Integrated Pathology Research Facility, Genomics Sequencing Facility, and Bio-Imaging and Analysis Facility.
Funding sources include the National Institutes of Health (R01GM079428) and the National Science Foundation (2114950).
SOURCE Cincinnati Children's Hospital Medical Center






Share this article